FROM PAIN TO PLEASURE…………
Did you know...?
-
Hemorrhoids are one of the most common ailments
known.
-
More than half the population will develop
hemorrhoids, usually after age 30.
-
The average person suffers in silence for a long
period before seeking medical care.
-
Today's treatment methods make some types of
hemorrhoid removal much less painful.
-
Some famous people i.e. Napoleon Bonaparte(emperor
of France),Fumimaro Konoye ( former prime minister
of Japan),Jimmy Carter (39thPresident of United
States)suffered from piles
What are hemorrhoids?
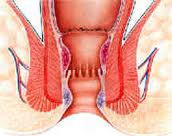
Often described as "varicose veins of the anus and
rectum", hemorrhoids are dilated and swollen cushions
(pads of tissue) in the anal canal, they may project
into the anal canal to form visible swellings. There are
two types of Hemorrhoids external and internal, which
refer to their location.
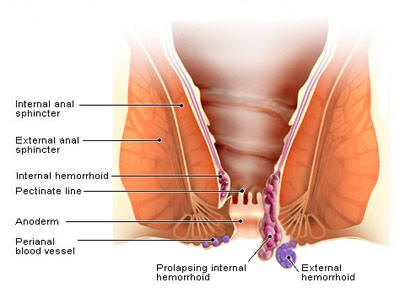
External (outside) hemorrhoids develop near the anus and
are covered by very sensitive skin.
Internal (inside) hemorrhoids develop within the anus
beneath the anal lining.
What causes hemorrhoids?
An exact cause is unknown; however, the upright
posture of humans alone forces a great deal of pressure
on the rectal veins, which sometimes causes them to
bulge. Other contributing factors include:
• Aging
• Chronic constipation or diarrhea
• Pregnancy
• Heredity
• Straining during bowel movements
• Faulty bowel function due to overuse of laxatives or
enemas
• Spending long periods of time (e.g., reading) on the
toilet
Whatever the cause, the tissues supporting the vessels
stretch. As a result, the vessels dilate; their walls
become thin and bleed. If the stretching and pressure
continue, the weakened vessels protrude.
What are the symptoms?
Painless bleeding and protrusion during bowel
movements, itching in the anal area are the most common
symptom. However, an internal hemorrhoid can cause
severe pain if it is completely "prolapsed" - protrudes
from the anal opening and cannot be pushed back inside.

Four degree of
hemorrhoids
First-degree hemorrhoids: Hemorrhoids that bleed
but do not prolapse.
Second-degree hemorrhoids: Hemorrhoids that
prolapse and retract on their own (with or without
bleeding).
Third-degree hemorrhoids: Hemorrhoids that
prolapse but must be pushed back in by a finger.
Fourth-degree hemorrhoids: Hemorrhoids that
prolapse and cannot be pushed back in.
How are hemorrhoids treated?
General measures (home care)
1. Anal Hygiene: Proper Cleaning techniques,
Avoid rubbing with toilet paper (This aggravates the
hemorrhoids and irritates the skin) Avoid prolonged
sitting or excessive straining while on the toilet
2. Diet: Take High Fiber Diet, beans, whole
grains, bran cereals, fresh fruits, and vegetables.
Limit food that have little or no fiber such as ice
cream, cheese, meat, and processed foods. Avoid soda
beverages, citrus juices, beer and wine, and caffeinated
products. Drink 8-10 glasses of water regularly
3. Hot Sitz Bath: Fill up your bathtub with warm
water and sit in it for 10-15 minutes.
Generally constipation and straining for bowel movements
promote piles (hemorrhoids) and hard stools can
traumatize existing hemorrhoids. Therefore, Mild
symptoms can be treated by increasing fluid and fiber
intake in the diet, along with eliminating straining
factors
Surgical Treatment
1. Ligation - the rubber band treatment - works
on internal hemorrhoids that protrude with bowel
movements. A small rubber band is placed over the
hemorrhoid, cutting off its blood supply. This procedure
sometimes produces discomfort and bleeding and may need
to be repeated for a full effect.
2. Injection and Coagulation - can also be used
on bleeding hemorrhoids that do not protrude. But
multiple sessions may be required.
3. Laser, infrared, or bipolar coagulation -
These methods involve the destruction of internal
haemorrhoids with laser or infrared light or heat.
Coagulation causes the haemorrhoidal tissue to harden
and degenerate, and to form scar tissue as the area
heals. Technique called Haemorrhoidolysis.
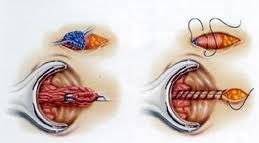
4. Conventional or open Surgical Method - Surgery
to remove haemorrhoids is called haemorrhoidectomy.. It
involves the surgical removal of excess haemorrhoidal
tissue and anal canal lining. Most anal surgeries are
being done under general or regional anaesthesia. Most
patients experience some degree of pain following the
surgery. It is painful for 7-10 days afterwards. While
surgery usually relieves the pain, swelling, bleeding,
and itching caused by haemorrhoids, a drawback to this
procedure is that the incisions are made in a highly
sensitive area and might require stitches, which can
cause the area to be tender and painful.
5. New Method or stapler haemorrhoidectomy (MIPH) -
In the past, open surgery was the only option
available to surgeons when they needed to see inside a
patient's body or remove or repair and organ. But today,
minimally invasive technology is completely changing the
way doctors approach patient care. While conventional
surgical haemorrhoidectomy is a safe and reliable
procedure, it is often associated with significant
postoperative pain. A new procedure for removing large
haemorrhoids, the stapler haemorrhoidectomy, is less
painful and allows patients to return to work and other
normal activities much earlier than with the
conventional procedure. Stapled Piles Surgery is also
known as PPH (procedure for prolapse and haemorrhoids)
or MIPH (Minimally invasive procedure for haemorrhoids).
This technique uses a stapling device and takes
advantage of the fact that pain-sensing nerve fibres are
absent higher in the anal canal. In this procedure, the
mucosa above the dentate line, which contains part of
the pile mass, is excised and stapled with the stapler
gun, thus taking care of bleeding and prolapse - the two
major components of piles. The pile masses are
compressed into a cup like cavity inside the stapler.
When fired, the titanium staples cut and seal
simultaneously, thus causing minimal bleeding and as the
cut line is above the nerves, there is reduction in post
operative pain. Additionally there is no incision on the
perianal skin or lower part of anal canal and the wound
in the anal mucosa is also primarily closed with a
stapler, thus, there is no need to do any post operative
dressing. It can be done as an outpatient, using local
anaesthesia with intravenous (IV) sedation. But it
should be done by a surgeon who is especially trained in
doing stapler surgery. This is because there are few
risks associated with the unskilled hands. The risks
include: damage to the rectal wall, overstretching of
sphincter muscles. etc.
Advantages of MIPH (Minimally invasive procedure for
haemorrhoids).
-
Smaller incisions resulting in reduced pain and
discomfort
-
Minimal scarring
-
Greater surgical precision
-
Fewer complications
-
Less blood loss and a decreased need for blood
transfusions
-
Reduced risk of infection
-
Shorter hospital stays
-
Faster recoveries
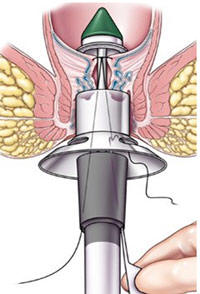

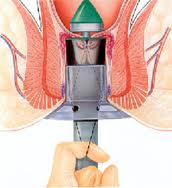
Prolapsed piles pulled into stapler
Post-operative picture show distance b/w dentate line &
staple line
Others: Doppler Guided Haemorrhoidal Artery Ligation (DG
HAL) and Recto-Anal Repair (HAL RAR) or Hemorrhoid
Artery Ligation operation (HALO) is a new FDA approved
operation
Do hemorrhoids lead to cancer?
No. There is no relationship between hemorrhoids and
cancer. However, the symptoms of hemorrhoids,
particularly bleeding, are similar to those of
colorectal cancer and other diseases of the digestive
system. Therefore, it is important that all symptoms are
investigated by a physician specially trained in
treating diseases of the colon and rectum .Don’t rely on
over-the-counter medications or other self-treatments.
DR VIVEK SINGLA
Gen. & Minimal invasive surgeon
MO. 9417377858
![]() HOME
| PROFILE
| PREGNANCY
|
INFERTILITY
| LAPARASCOPY
| PHOTO
GALLERY | CONTACT US
HOME
| PROFILE
| PREGNANCY
|
INFERTILITY
| LAPARASCOPY
| PHOTO
GALLERY | CONTACT US