What is the Gallbladder?
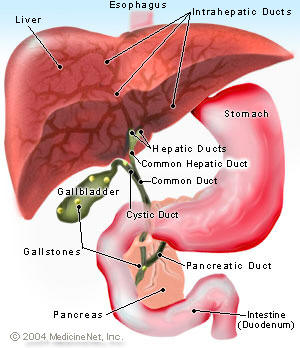
The gallbladder is a pear-shaped structure that is found
attached to the liver. The bile duct is a tube that
transports bile from the liver to the small intestine.
The gallbladder is attached to the bile duct by a small
tube called the cystic duct. Bile is collected in the
gallbladder between meals and empties into the bile duct
through the cystic duct during a meal.
What is the bile duct?
The bile duct is long tube-like structure that connects
the liver to the intestine. The liver makes bile that is
required for the digestion of food. The bile from the
liver is transported to the intestine by the bile duct.
The top half of the bile duct is associated with the
liver while the bottom half of the bile duct is
associated the pancreas through which it passes on its
way to the intestine. It opens in the part of the
intestine called the duodenum into a structure called
the Ampulla.
Blockage of the bile duct by a cancer or scarring from
injury prevents the bile from being transported to the
intestine and the bile accumulates in the blood. This
condition is called jaundice and the skin and eyes
becomes yellow from the accumulated bile in the blood.
This condition also causes severe itchiness.
Jaundice is commonly causes by conditions such as
pancreatic cancer caused by blockage of the bile duct
passing through the cancerous portion of the pancreas,
bile duct cancer, blockage by a stone in patients with
gallstones and from scarring after injury to the bile
duct during gallbladder removal.
What are gallstones?
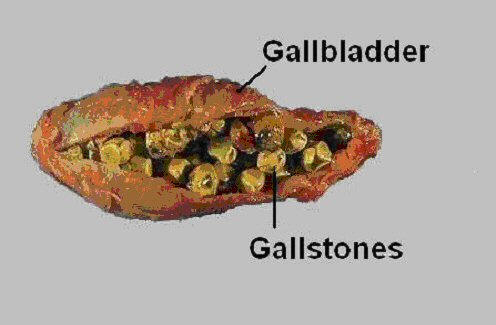 Gallstones
are stone-like substances that are found in the
gallbladder. There are two types of gallstones: pigment
stones and cholesterol stones. In the majority of
patients cholesterol stones are present. In many people
the cause for gallstones appears to be interaction
between hereditary causes and the diet. Certain
population groups such as the Latino population have a
an increase tendency to form gallstones.
Gallstones
are stone-like substances that are found in the
gallbladder. There are two types of gallstones: pigment
stones and cholesterol stones. In the majority of
patients cholesterol stones are present. In many people
the cause for gallstones appears to be interaction
between hereditary causes and the diet. Certain
population groups such as the Latino population have a
an increase tendency to form gallstones.
Gallstones are formed when the bile that is produced by
the liver becomes very enriched with fatty substances.
In the majority of patients with gallstones, the
gallbladder wall is abnormal due to many previous
episodes of inflammation. Removal of the stones only is
associated with rapid development of new stones in the
gallbladder.
What symptoms do gallstones cause?
Gallstone causes symptoms that are usually associated
with eating a fat rich meal. Many patients develop pain
in the right upper part of the abdomen that may last
from few minutes to few hours. Some patients complain of
indigestion, feeling fullness, and discomfort in the
upper part of the abdomen after a meal.
How are gallstones diagnosed?
Gallstones are diagnosed by a radiological test
called ultrasound. In this test the radiologist utilizes
an instrument that sends sound waves to the gallbladder.
The sound waves detect the stones, which are then seen
on the ultrasound. An ultrasound is an excellent test
for gallstones and diagnoses the stones in more than 98%
of all patients with gallstones.
What are the complications associated gallstones?
Gallstones can cause many serious complications.
Some of the complications that are caused by gallstones
include:
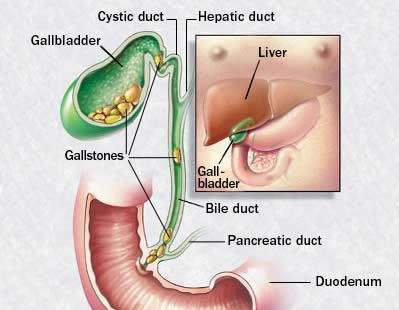
- Acute cholecystitis. In this condition a stone
blocks the cystic duct and therefore the gallbladder
cannot empty its content into the bile duct. The
secretions in the gallbladder accumulate and become
infected. Patients often develop a bad infection of the
gallbladder with severe pain in the upper part of the
abdomen, fevers, and other symptoms such as nausea and
vomiting. Patients usually require admission to the
hospital for treatment with antibiotics and emergent
removal of the gallbladder.
- Jaundice. Jaundice develops when a stone passes
from the gallbladder through the cystic duct into the
bile duct and blocks the bile duct. Patients present
with a yellowish discoloration of their skin associated
with severe itchiness. An emergency procedure by a
gastroenterologist is often required to remove the
stones from the bile duct.
- Acute pancreatitis. In some patients passage of
the stone from the gallbladder into the bile duct is
associated with injury to the pancreas. Pancreatitis is
one of the most severe complications of gallstones. Of
all patients that develop pancreatitis, 85% of the
patients get better very quickly however in 15% the
attack can be severe and lead to hospitalization that
may extend for many days to weeks in an intensive care
unit. Pancreatitis develops with severe pain in the
abdomen and back that is associated wit nausea,
vomiting, and fevers.
- Cancer of the gallbladder. In some patients when
gallstones are present over many years (usually more
than 15 years) there is an increase risk of cancer in
the gallbladder.
How are gallstones treated?
Gallstones are treated by removal of the gallbladder
by a procedure called cholecystectomy. Cholecystectomy
can be performed through an open surgical incision and
by laparoscopic surgery. In the past the gallbladder was
removed through an open surgical incision.
Laparoscopic cholecystectomy
Today the almost all gallbladder surgery is performed by
laparoscopic surgery. Laparoscopic gallbladder surgery
is associated with a shorter hospitalization, less pain
and discomfort after the surgery and a rapid recovery
allowing many patients to go back to work within a short
period of time after the surgery.
What is a laparoscopic cholecystectomy?
Laparoscopic cholecystectomy is a procedure in which
the gallbladder is removed by laparoscopic techniques.
Laparoscopic surgery also referred to as minimally
invasive surgery describes the performance of surgical
procedures with the assistance of a video camera and
several thin instruments.
During a laparoscopic surgical procedure, small
incisions of up to half an inch are made and plastic
tubes called ports are placed through these incisions.
The camera and the instruments are then introduced
through the ports which allow access to the inside of
the patient. The camera transmits an image of the organs
inside the abdomen onto a television monitor.The surgeon
is not able to see directly into the patient without the
traditional large incision. The video camera becomes a
surgeon’s eyes in laparoscopy surgery, since the surgeon
uses the image from the video camera positioned inside
the patient’s body to perform the procedure.
Benefits of minimally invasive or laparoscopic
procedures include less post operative discomfort since
the incisions are much smaller, quicker recovery times,
shorter hospital stays, earlier return to full
activities and much smaller scars. Furthermore, there
may be less internal scarring when the procedures are
performed in a minimally invasive fashion compared to
standard open surgery.
How safe is laparoscopic gallbladder surgery?
Laparoscopic cholecystectomy is a very safe
operation. The overall complication rate is less than
2%. The complication rate for laparoscopic gallbladder
surgery is similar to the complication rate for
traditional open gallbladder surgery when performed by a
properly trained surgeon.
How is laparoscopic cholecystectomy performed?
Many thousands of laparoscopic cholecystectomy have
been performed in the USA and this operation has an
excellent safety record. Some of the important steps in
the operation are as follows:
-
General anesthesia is utilized, so the patient is
asleep throughout the procedure.
-
An
incision that is approximately half an inch is made
around the umbilicus ( belly button), three other
quarter to half inch incisions are made for a total
of four incisions. Four narrow tubes called
laparoscopic ports are placed through the tiny
incisions for the laparoscopic camera and
instruments.
-
A
laparoscope (which is a long thin round instrument
with a video lens at its tip) is inserted through
the belly button port and connected to a special
camera. The laparoscope provides the surgeon with a
magnified view of the patient's internal organs on a
television screen.
-
Long
specially designed instruments are inserted through
the other three ports that allow your surgeon to
delicately separate the gallbladder from its
attachments to the liver and the bile duct and then
remove it through one of the ports from the abdomen.
-
Your
surgeon may occasionally perform an X-ray, called a
cholangiogram, to exam for stones in the bile duct.
-
After
the gallbladder is removed from the abdomen then the
small incisions are closed
What
happens if at surgery the surgeon cannot complete the
operation with laparoscopic techniques?
In a small number of patients if excessive scarring is
present or the anatomy of the structures is not clear
then for safety reasons the surgeon may decide too
convert the operation to an open surgical operation
through a traditional large surgical incision. Less than
5% of all laparoscopic cholecystectomy procedures are
converted to open procedures.
The decision to convert to an open operation is strictly
based on patient safety. Factors that may increase the
risk of converting to the "open" procedure include
obesity, a history of prior abdominal surgery causing
dense scar tissue, acute cholecystitis or bleeding
problems during the operation.
What are the risks of laparoscopic gallbladder
surgery?
Complications of a laparoscopic cholecystectomy are
infrequent and the vast majority of laparoscopic
gallbladder patients recover and quickly return to
normal activities. Some of the complications that can
occur include bleeding, infection, leakage of bile in
the abdomen, pneumonia, blood clots, or heart problems.
Surgical injury to an adjacent structures such as the
common bile duct, duodenum or the small intestine may
occur rarely and may require another surgical procedure
to repair it. If the gallbladder is accidentally or
deliberately opened during the procedure stones may fall
out of the gallbladder and in to the abdomen that may
give rise to later scarring.
How long will you be in the hospital?
Once a diet is tolerated, patients leave the
hospital. Most patients go home the next day after a
laparoscopic cholecystectomy. Some may even go home the
same day the operation is performed. This compares with
a five day stay following the open cholecystectomy
procedure.
What is the recovery period and how soon can you go
back to work?
Patients will probably be able to get back to normal
activities within a week's time, including driving,
walking up stairs, light lifting and work. Activity is
dependent on how the patient feels. Walking is
encouraged. Patients can remove the dressings and shower
the day after the operation. In general, recovery should
be progressive, once the patient is at home.
Most patients are fully recovered and may go back to
work after seven days.
Often, this depends on the nature of your job since
patients who perform manual labor or heavy lifting may
require two to four weeks of recovery.
What should you be concerned about after going home?
The development of fever, yellow skin or eyes,
worsening abdominal pain, distention, persistent nausea
or vomiting, or drainage from the incision are
indications that a complication may have occurred. You
should contact your surgeon under these circumstances.
![]() HOME
| PROFILE
| PREGNANCY
|
INFERTILITY
| LAPARASCOPY
| PHOTO
GALLERY | CONTACT US
HOME
| PROFILE
| PREGNANCY
|
INFERTILITY
| LAPARASCOPY
| PHOTO
GALLERY | CONTACT US